Varicose veins are a common vascular condition that affects millions of people worldwide. These veins, often appearing swollen, twisted, and blue or dark purple, are typically found in the legs and can cause discomfort, pain, and cosmetic concerns. Understanding what is a varicose vein, how it develop, and the available treatment options is essential for managing this condition effectively.
Anatomy of Veins
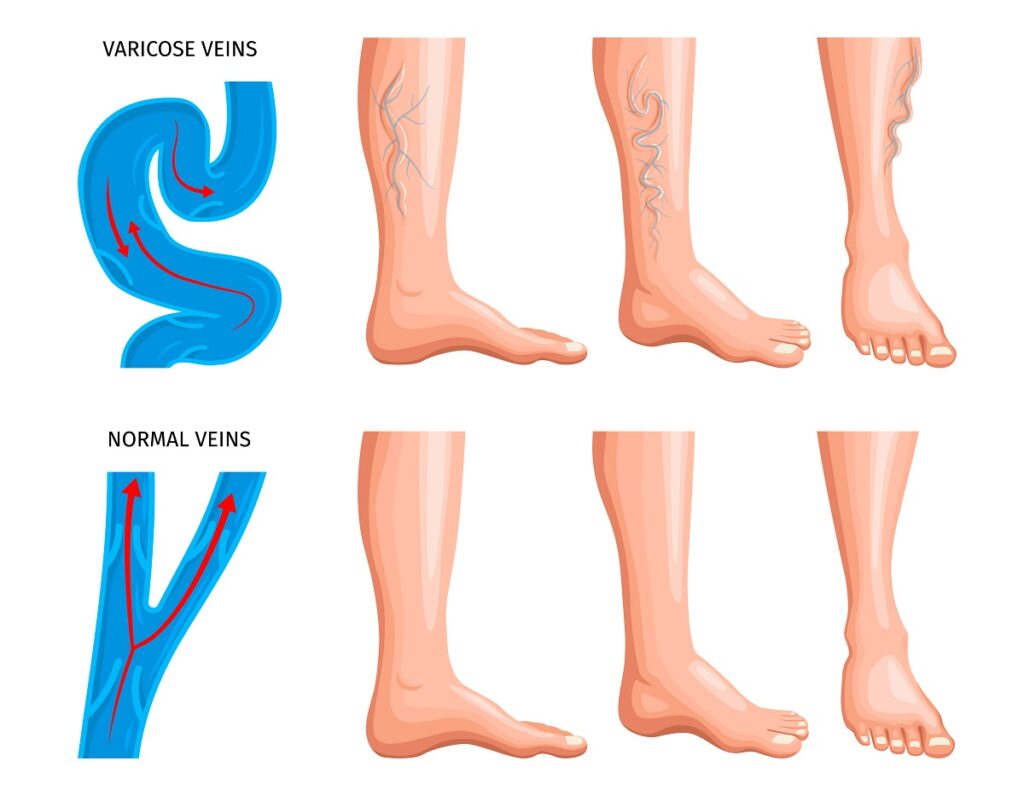
To comprehend varicose veins, it’s important to understand the basic anatomy and function of veins. Veins are blood vessels responsible for returning deoxygenated blood from various parts of the body back to the heart. They have a series of one-way valves that prevent blood from flowing backward, ensuring efficient circulation.
In the legs, there are two main types of veins: superficial veins and deep veins. Superficial veins lie close to the skin’s surface, while deep veins are located deeper within the muscles. Connecting these two systems are perforator veins, which help transfer blood from the superficial to the deep veins.
Pathophysiology of Varicose Veins
Varicose veins develop when the valves within the veins become weakened or damaged, leading to the pooling of blood. This condition, known as venous insufficiency, causes increased pressure within the veins, which can result in the veins becoming enlarged, twisted, and varicose.
Several factors contribute to the development of varicose veins:
- Genetics: A family history of varicose veins increases the likelihood of developing the condition. Genetic factors can influence the strength and structure of vein walls and valves.
- Age: Aging is a significant risk factor, as veins lose elasticity and valves weaken over time. This natural wear and tear can lead to venous insufficiency.
- Gender: Women are more prone to varicose veins than men, partly due to hormonal changes during pregnancy, menstruation, and menopause, which can relax vein walls.
- Pregnancy: The increased blood volume and pressure on the veins in the pelvis and legs during pregnancy can contribute to the development of varicose veins. Additionally, hormonal changes can relax vein walls.
- Obesity: Excess body weight puts additional pressure on the veins, especially in the legs, increasing the risk of varicose veins.
- Prolonged Standing or Sitting: Occupations or lifestyles that involve long periods of standing or sitting can hinder blood flow, leading to increased venous pressure and the development of varicose veins.
- Inactivity: Lack of physical activity can weaken the muscles that help pump blood back to the heart, contributing to venous insufficiency.
Symptoms and Complications
Varicose veins can manifest with various symptoms, ranging from mild cosmetic concerns to significant discomfort and complications. Common symptoms include:
- Visible, Twisted Veins: The most apparent sign of varicose veins is the appearance of enlarged, twisted, and discolored veins, usually on the legs.
- Pain and Aching: Many individuals with varicose veins experience aching, throbbing, or a heavy feeling in the affected legs, especially after prolonged standing or sitting.
- Swelling: Swelling in the lower legs and ankles is a common symptom, particularly towards the end of the day.
- Itching and Skin Changes: The skin around varicose veins may become dry, itchy, and thin. In severe cases, it can lead to dermatitis or eczema.
- Muscle Cramping: Some people experience muscle cramps, particularly at night, which can be attributed to poor circulation.
- Restless Legs: Varicose veins can contribute to restless legs syndrome, causing an uncontrollable urge to move the legs.
In addition to these symptoms, varicose veins can lead to more serious complications:
- Venous Ulcers: Chronic venous insufficiency can result in the development of painful, non-healing ulcers, typically around the ankles.
- Blood Clots: Varicose veins increase the risk of superficial thrombophlebitis (inflammation and clotting in the veins just below the skin) and deep vein thrombosis (DVT), a more serious condition where clots form in the deep veins.
- Bleeding: Varicose veins close to the skin surface can sometimes rupture, leading to significant bleeding.
What is a Varicose Vein and How to Diagnose it
Diagnosing varicose veins typically involves a physical examination and a review of the patient’s medical history. Healthcare providers may also use diagnostic tests to assess the severity of the condition and rule out other potential issues. Common diagnostic methods include:
- Doppler Ultrasound: This non-invasive test uses sound waves to visualize blood flow in the veins and detect any abnormalities, such as valve dysfunction or blood clots.
- Venogram: In some cases, a venogram may be performed, where a contrast dye is injected into the veins, allowing X-rays to provide detailed images of the vein structure.
Treatment Options for Varicose Veins
The treatment of varicose veins aims to alleviate symptoms, prevent complications, and improve the appearance of the affected veins. Several treatment options are available, ranging from conservative measures to minimally invasive procedures and surgery:
Lifestyle Modifications:
Making certain lifestyle changes can help manage varicose veins and prevent their progression. These include:
- Regular Exercise: Physical activity, such as walking, swimming, or cycling, can improve circulation and strengthen leg muscles.
- Weight Management: Maintaining a healthy weight reduces pressure on the veins and lowers the risk of varicose veins.
- Elevating Legs: Elevating the legs when resting can help reduce swelling and improve blood flow.
- Avoiding Prolonged Standing or Sitting: Taking breaks to move around and change positions can prevent blood from pooling in the veins.
Compression Stockings:
Compression stockings are specially designed garments that apply graduated pressure to the legs, helping to improve blood flow and reduce swelling. They are available in various strengths and styles and are often recommended as a first-line treatment.
Sclerotherapy:
Sclerotherapy is a minimally invasive procedure in which a solution is injected directly into the varicose veins. This solution irritates the vein walls, causing them to collapse and eventually fade. Sclerotherapy is effective for smaller varicose veins and spider veins.
Endovenous Laser Treatment (EVLT):
EVLT is a minimally invasive procedure that uses laser energy to heat and close off the affected vein. A thin laser fiber is inserted into the vein under ultrasound guidance, and the laser energy is applied, causing the vein to seal shut. Blood is then rerouted to healthier veins.
Radiofrequency Ablation (RFA):
Similar to EVLT, RFA uses radiofrequency energy to heat and close off the varicose vein. A catheter is inserted into the vein, and radiofrequency energy is applied to seal the vein. This procedure is effective for larger varicose veins.
Vein Stripping and Ligation:
Vein stripping is a surgical procedure where the affected vein is removed through small incisions. It is typically reserved for severe cases or when other treatments have not been successful. Ligation involves tying off the vein to prevent blood flow.
Ambulatory Phlebectomy:
This procedure involves the removal of smaller varicose veins through tiny incisions in the skin. It is performed under local anesthesia and is suitable for superficial veins.
Laser or Intense Pulsed Light (IPL) Therapy:
Laser or IPL therapy is used to treat spider veins and smaller varicose veins. These treatments use light energy to target and collapse the veins, causing them to fade over time.
Prevention for Varicose Veins
While it’s not always possible to prevent varicose veins, certain measures can reduce the risk of developing them or minimize their severity:
- Regular Exercise: Engaging in regular physical activity helps improve circulation and maintain healthy veins.
- Healthy Diet: Eating a balanced diet rich in fiber and low in salt can help prevent constipation and reduce pressure on the veins.
- Weight Management: Maintaining a healthy weight reduces the strain on the veins and lowers the risk of varicose veins.
- Leg Elevation: Elevating the legs periodically can help reduce swelling and improve blood flow.
- Compression Stockings: Wearing compression stockings can provide additional support to the veins and improve circulation.
- Avoiding Tight Clothing: Tight clothing can restrict blood flow and contribute to varicose veins. Opt for loose-fitting clothes that do not constrict the waist, groin, or legs.
- Regular Movement: Avoiding prolonged periods of sitting or standing can prevent blood from pooling in the veins. Take breaks to move around and stretch.
Conclusion
Varicose veins are a common condition that can cause discomfort, pain, and cosmetic concerns. Understanding what is a varicose vein, it’s symptoms, and treatment options is essential for managing this condition effectively. While lifestyle modifications, compression stockings, and minimally invasive procedures can provide relief for many individuals, severe cases may require surgical intervention. By adopting preventive measures and seeking appropriate treatment, individuals with varicose veins can improve their quality of life and reduce the risk of complications. If you suspect you have varicose veins or are experiencing symptoms, it is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.